Resource Guide: 5 Hot Topics in Telebehavioral Health & SUD Treatment
Webinar: 11/4/2021
Prepared by innovaTel Telepsychiatry and Foley & Lardner


Learn how innovaTel can help you help your patients
Fill out the form and receive our latest whitepaper in your inbox.
About innovaTel Telepsychiatry
Founded by a clinical team with 30+ years of experience
CMHC Roots
Prior to innovaTel, its founder started the first CMHC in NW Pennsylvania, developing a successful telepsychiatry program through a small SAMSHA grant.
Meet a Need
Recruitment and retention of psychiatric providers was a constant challenge for the clinic.
Telepsychiatry Success
Word of the clinic’s adoption of and success with its telepsychiatry model spread quickly throughout the country.
innovaTel Begins
As a result of the model’s success, innovaTel was founded in April of 2014.

Improved Access, Improved Outcomes
- We understand that workforce development challenges are affecting delivery of care and we are committed to helping organizations grow their treatment teams through our telehealth partnerships.
- innovaTel is a clinically owned and operated national telehealth company that was founded with a mission to increase access to behavioral health treatment.
- We customize all of our telehealth partnerships based on the needs of the organizations that we partner with, so today’s goal is to really get to know your organization better so that we can understand if we may be a good partner for you.
- Ultimately, with our partnerships your team would get to interview and choose providers that become a virtual member of your team, it’s our goal that these providers are just as much a part of the team as if they were there on site, the only difference being that they connect virtually.
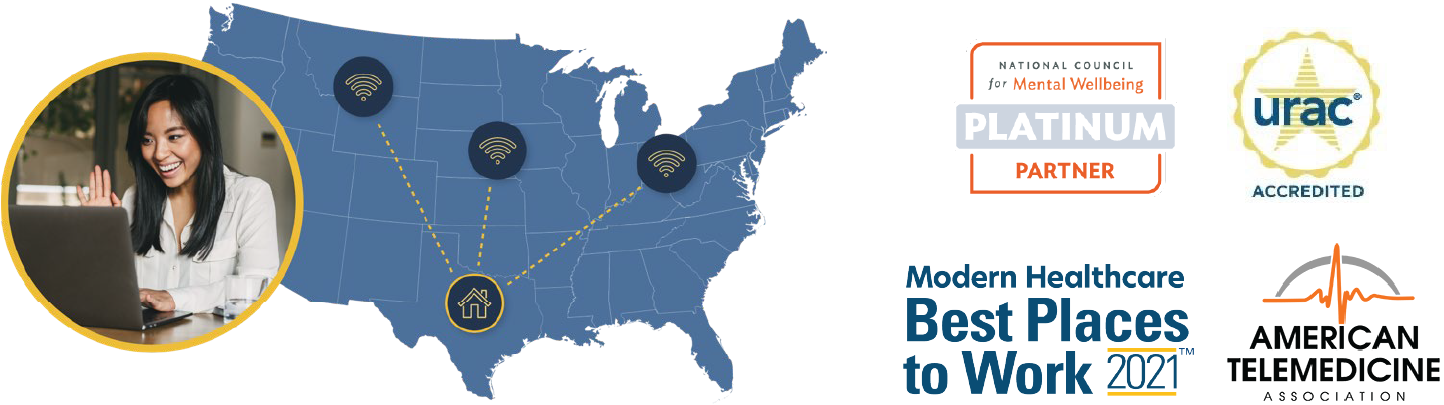
Increased Demand for BH Services
Nationally, we are seeing an increase in demand for behavioral health treatment.
Historically, experts have estimated that 1 in 5 adults in the U.S. may be in need of behavioral health services. New estimates predict an increased need, as 1 in 3 may need services, which equates to an additional 35 million people.
~35M
Additional people may experience BH conditions, including 1.6M directly affected by COVID illness or loss.
1 in 3
could have a BH need in 2021.
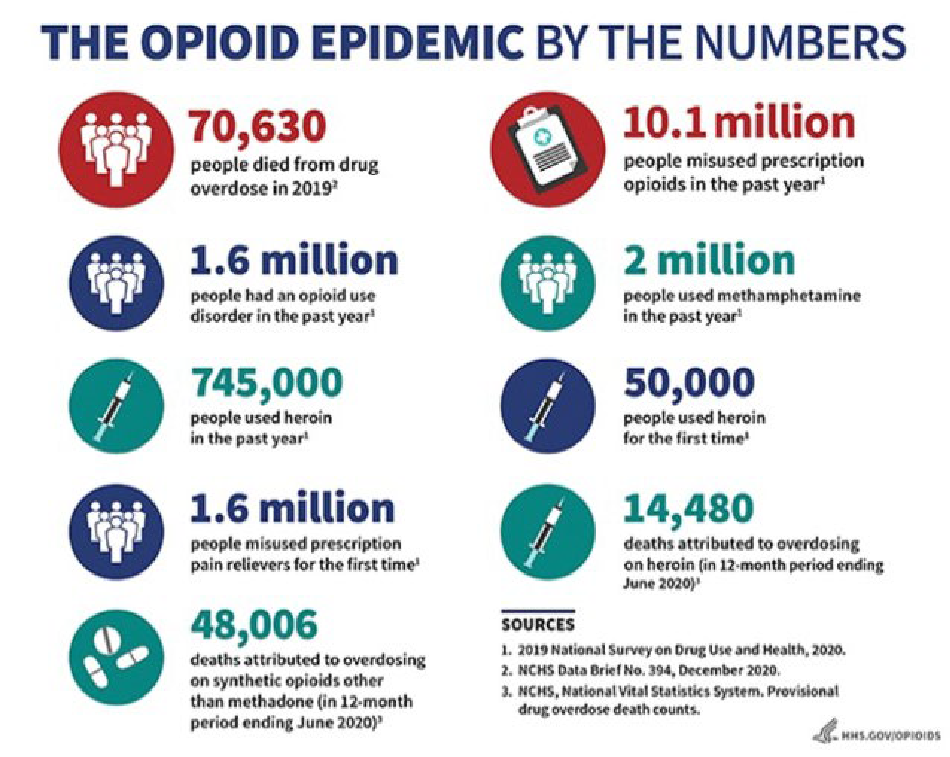
U.S. Opioid Epidemic
- More than 136 people a day die from opioid-related drug overdoses
- SUD: Substance Use Disorder Treatment
- OUD: Opioid Use Disorder Treatment
Tools to Combat OUD: MAT
- Medication-assisted treatment (MAT) is the use of medications, in combination with counseling and behavioral therapies, to provide a “whole-patient” approach to the treatment of substance use disorders.
- Medications used in MAT are approved by the Food and Drug Administration (FDA) and MAT programs are clinically driven and tailored to meet each patient’s needs.
- FDA has approved several different medications to treat alcohol and opioid use disorders MAT medications relieve the withdrawal symptoms and psychological cravings that cause chemical imbalances in the body.
- Alcohol Use Disorder (AUD): Acamprosate, disulfiram, and naltrexone
- Opioid Overdose: Naloxone
- Opioid Dependency: Buprenorphine, methadone, naltrexone

Oversight of SUD MAT Treatment
Federal Regulation
- Methadone and Buprenorphine = controlled substances
- Drug Enforcement Administration (DEA), Diversion Control Division
- Registration, prescribing controlled substances (including remote prescribing)
- Substance Abuse and Mental Health Services Administration (SAMHSA)
- Fed. Controlled Substances Act and Regulations
SUD MAT
State Regulation
- (1) a level (i.e., group licensure, certification, or registration requirements) and
- (2) an individual practitioner level (i.e., specific buprenorphine prescribing guidelines), controlled substance prescribing requirements
- State Opioid Treatment Authorities

Use of Telemedicine for OUD Treatment
- Remote Prescribing
- Ryan Haight Act
- State Law on Controlled Substance Prescribing and Buprenorphine Treatment
- State Licensure (provider and program)
- Telehealth Practice Standards
COVID-19 Waivers – Prescribing
Federal
- Ryan Haight Act (21 U.S.C.829))
- DEA Registration
- MAT Telehealth (modality)
State
- State by State controlled substance prescribing waivers
- State MAT Prescribing Waivers
- Modality Requirements


Federal Ryan Haight Act
Pre-COVID
- Ryan Haight Act: 21 U.S.C. 829(e)
- Requires a prior in-person examination in order to issue a “valid prescription” for a controlled substance
- Exceptions
COVID Waivers
- Public Health Emergency Exception 42 U.S.C. 247d (Jan. 31, 2020)
- Prescription is issued for a legitimate medical purpose by a practitioner acting in the usual course of his/her professional practice
- Audio-visual, real-time, two-way interactive communication system; and
- The practitioner is acting in accordance with applicable Federal and State laws.
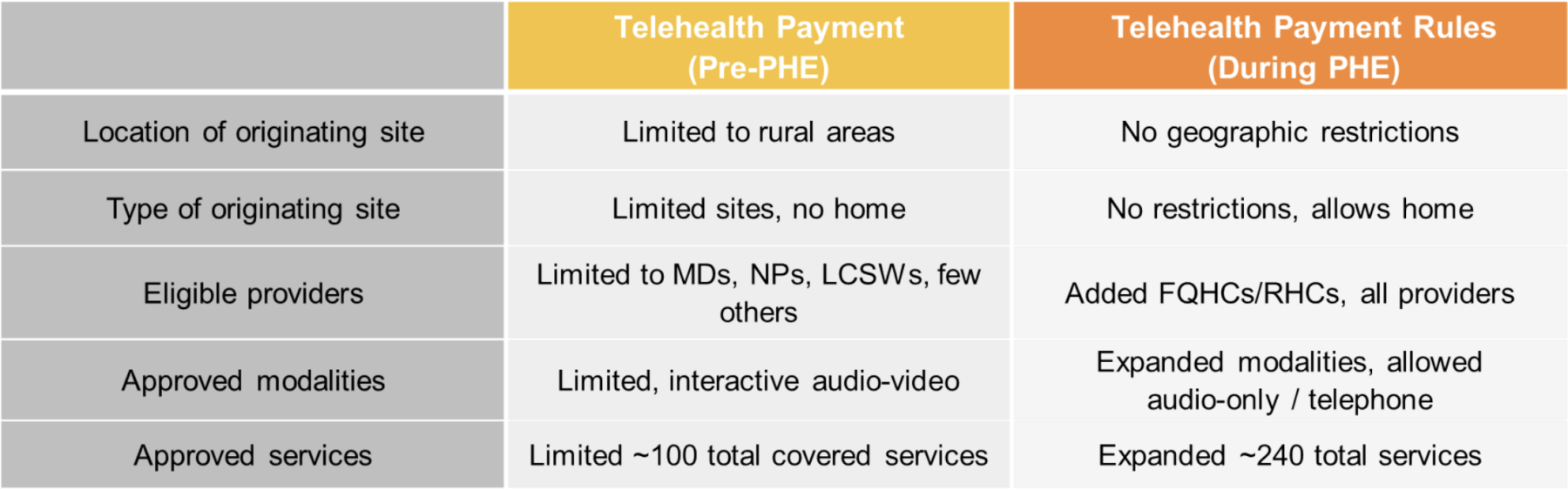
Medicare Telehealth Reimbursement Policies
Pre-PHE and Today
Telebehavioral Health Payment
Opportunities
Many telebehavioral health and OUD telehealth services are billable under Medicare and other payers
- Psychiatric diagnostic evaluation codes
- Psychiatric crisis codes
- Individual and group therapy codes
- Office E/M codes for new and established patients
- Office-based opioid treatment codes
- ED and initial inpatient hospital and SNF consultation codes
- Home visits for established patients w/SUD


Telebehavioral Health Reimbursement
2022 Medicare Physician Fee Schedule Final Rule
Key Policy Changes
- Expands telemental health services, Section 123, Consolidated Appropriations Act of 2020 (CAA)
- Removes rural geographic restriction on originating sites
- Adds patient’s home as eligible originating site
- Amends definition of telehealth (e.g.,a live interactive audio-video encounter) to allow use of audio-only or telephone modalities for telemental health services to the patient at home, under certain conditions
- Requires prior in-person visit, subsequent annual visit w/allowed exception
- Clarifies mental health services can include services for treatment of SUDs
- Effective after PHE
- Allows FQHCs & RHCs to furnish telemental health services including via video or audio-only telephone modalities, requires in-person annual visit w/allowed exception
- Allows Opioid Treatment Programs (OTPs) to furnish therapy and counseling services through audio-only modalities after PHE, under certain conditions
During PHE
- Broad expansion of coverage and reimbursement to drive adoption of telehealth
- Added the patient’s home as eligible originating site
- Added audio-only / telephone as eligible modality
- Expanded providers who could furnish and bill telehealth services
- Removed licensing and other telehealth requirements
Today
- Some state emergencies have expired, extending flexibilities for certain services
- States amending Medicaid telehealth laws to add eligible providers (e.g. FQHCs/RHCs), home and schools as originating sites, audio-only modalities and telehealth services
- States adding payment and audio-only language to commercial payer telehealth laws
- States joining interstate licensure compacts